Duloxetine HCl CAS NO 136434-34-9 Inquire about Duloxetine HCl
Tecoland supplies Duloxetine HCl bulk active pharmaceutical ingredient (API) to the pharmaceutical industry. Our Duloxetine HCl is manufactured by cGMP compliant facility. Welcome to contact us for further details including current DMF status for the product and up to date regulatory status of the manufacturing facility. We look forward to assisting you with your research and development projects.
What is Duloxetine?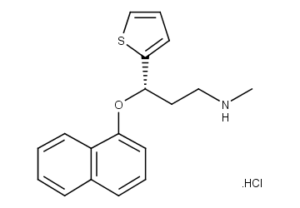
Duloxetine (sold under the brand names Cymbalta, Ariclaim, Xeristar, Yentreve, Duzela) is a serotonin-norepinephrine reuptake inhibitor (SNRI) manufactured and marketed by Eli Lilly. It is effective for major depressive disorder and generalized anxiety disorder (GAD). Duloxetine failed the US approval for stress urinary incontinence amidst concerns over liver toxicity and suicidal events; however, it was approved for this indication in Europe, where it is recommended as an add-on medication in stress urinary incontinence instead of surgery. It can also relieve the symptoms of painful peripheral neuropathy, particularly diabetic neuropathy, and it is used to control the symptoms of fibromyalgia.
Medical uses
The main uses of duloxetine are in major depressive disorder, general anxiety disorder, stress urinary incontinence, painful peripheral neuropathy, fibromyalgia, and chronic musculoskeletal pain associated with osteoarthritis and chronic lower back pain. It is being studied for various other indications.
Major depressive disorder
Duloxetine has demonstrated efficacy for the treatment of major depressive disorder. Recently, duloxetine was shown to be effective in elderly with recurrent major depressive disorder where it improved cognition, depression, and some pain measures.
Stress urinary incontinence
Duloxetine was first reported to improve outcomes in stress urinary incontinence (SUI) in 1998. Systematic reviews with meta-analysis, conducted in 2005 by Cochrane Collaboration and in 2008 by University of Minnesota, concluded that duloxetine failed to cure SUI better than placebo. According to the Cochrane review, some studies showed that episodes of incontinence were reduced by about 50%. This was associated with an improvement in quality of life measurements. According to the University of Minnesota review, duloxetine performed worse than oxybutynin (Ditropan) or tolterodine (Detrol) that cured 18% of the cases, or than pelvic floor muscle training + bladder training, which cured 13% of the cases. In terms of “improvement”, that is incomplete cure, duloxetine showed improvement in 11% of patients while pelvic floor muscle training + bladder training showed improvement in 36% of the cases. Significant side effects were common with duloxetine; they were reported as acceptable and about a fifth had to discontinue the medication because of poor tolerance.
In addition, the full report prepared by Minnesota Evidence-based Practice Center for the U.S. government, on which the University of Minnesota review is based, notes that weight reduction would result in improved SUI in 990 adults per 1,000 treated. In the light of the cited data, the report does not mention duloxetine in its policy recommendations. The only recommended interventions are early behavioral changes in weight, physical activity, and pelvic floor muscle training.
The only clinical trial, which directly compared duloxetine with the gold standard of the SUI treatment pelvic floor muscle training (PFMT) was conducted by Eli Lilly and gave mixed results. The incontinence episode frequency in duloxetine group decreased by 57% vs. 35% in the PFTM group. However, the differences in the pad use and quality of life were not statistically significant. To the contrary, 65% patients doing PFTM reported feeling better vs 54% of the patients on duloxetine. 31% of the patients on duloxetine discontinued the trial due to the side effects during the first 12 weeks. In the continuation of this trial more than 91% of the patients on duloxetine experienced side effects.
Summing up the existing evidence, a review in Prescrire International recommends pelvic floor exercises, which are “risk-free and effective in two-thirds to three-quarters of cases”, as the first line treatment of SUI. Duloxetine use reduced the frequency of stress incontinence by one episode a day as compared with placebo. “The tangible effect of duloxetine on the quality of life is doubtful, with a maximum gain of five points on a 100-point scale.” The review notes that, at best, duloxetine efficacy is “modest and transient, while its adverse effects are numerous and potentially severe.”
Diabetic peripheral neuropathy
Duloxetine was approved for the pain associated with diabetic peripheral neuropathy (DPN) based on the positive results of two clinical trials. The average daily pain was measured using 11-point scale, and duloxetine treatment resulted in an additional 1¨C1.7 points decrease of pain as compared with placebo. At least 50% pain relief was achieved in 40¨C45% of the duloxetine patients vs. 20¨C22% of placebo patients. The pain almost completely disappeared, decreasing by more than 90%, in 9¨C14% of duloxetine patients vs. 2¨C4% of placebo patients. Most of the response was achieved in the first two weeks on the medication. Duloxetine slightly increased the fasting serum glucose; however this effect was deemed to be of “minimal clinical significance”.
Duloxetine was not effective for the numbness or tingling, nor for the other complications of diabetes. It reduced the pain without treating the underlying nerve damage. Only tight glycemic control was unequivocally demonstrated to slow the progression of neuropathy. Benfotiamine, alpha-lipoic acid, and ranirestat have also shown some promise.
The comparative efficacy of duloxetine and established pain-relief medications for DPN is unclear. An independent systematic review in BMJ noted that tricyclic antidepressants (imimpramine and amitriptyline), traditional anticonvulsants and opioids have better efficacy than duloxetine. Duloxetine, tricyclic antidepressants and anticonvulsants have similar tolerability while the opioids caused more side effects. A review in Drug and Therapeutic Bulletin saw no place for duloxetine in the treatment of DPN, based on its high cost and insufficient evidence of the comparative efficacy with tricyclic antidepressants. Another independent review in Prescrire International, considered the moderate pain relief achieved with duloxetine to be clinically insignificant and the results of the clinical trials¡ªunconvincing. The reviewer saw no reason to prescribe duloxetine in practice. The comparative data collected by reviewers in BMC Neurology indicated that amitriptyline, other tricyclic antidepressants and venlafaxine may be more effective. However, the authors noted that the evidence in favor of duloxetine is much more solid.
Generalized anxiety disorder
Duloxetine is as effective as venlafaxine in the treatment of generalized anxiety disorder with demonstrated improvements in function and quality of life for sufferers. Long-term use of duloxetine prevents relapse of generalized anxiety disorder. Although this view was repeated in a recent independent review, the major guidelines such as Maudsley Prescribing Guidelines, Mayo Clinic Health Information and Canadian Psychiatric Association Guidelines do not mention duloxetine among the recommended treatment options.
Disclaimer:
Information on this page is provided for general information purposes. You should not make a clinical treatment decision based on information contained in this page without consulting other references including the package insert of the drug, textbooks and where relevant, expert opinion. We cannot be held responsible for any errors you make in administering drugs mentioned on this page, nor for use of any erroneous information contained on this page.